Tularemia
Posted on 10 April 2023.
Tularemia is a febrile disease caused by the gram-negative bacteria Francisella tularensis; it may resemble typhoid fever. Symptoms are a primary local ulcerative lesion, regional lymphadenopathy, profound systemic symptoms, and, occasionally, atypical pneumonia. Diagnosis is primarily epidemiologic and clinical and supported by serologic tests. Treatment is with streptomycin, gentamicin, chloramphenicol, ciprofloxacin, or doxycycline.
There are 7 clinical syndromes associated with tularemia,clinical manifestations vary by the type of exposure to the organism.
The causative organism, F. tularensis, is a small, pleomorphic, nonmotile, nonsporulating aerobic bacillus that enters the body by;
Ingestion of contaminated food or water
Bite of an infected arthropod vector (ticks, deer flies, fleas)
Inhalation
Direct contact with infected tissues or material
Tularemia does not spread from person to person.
Types of Tularemia
The organism can penetrate apparently unbroken skin but may actually enter through microlesions.
Two types of F. tularensis cause most cases of tularemia:
Type A: This type is a more virulent serotype for humans; it usually occurs in rabbits and rodents in the US and Canada.
Type B: This type usually causes a mild ulceroglandular infection and occurs in water and aquatic animals in Europe and Asia.
Hunters, butchers, farmers, and fur handlers are most commonly infected. In winter months, most cases result from contact (especially during skinning) with infected wild rabbits. In summer months, infection usually follows handling of other infected animals or birds or bites of infected ticks or other arthropods. Rarely, cases result from eating undercooked infected meat, drinking contaminated water, or mowing fields in endemic areas. In the Western states, ticks, deer flies, horse flies, and direct contact with infected animals are other sources of infection. Human-to-human transmission has not been reported. Laboratory workers are at particular risk because infection is readily acquired during normal handling of infected specimens.
Tularemia is considered a possible agent of bioterrorism because inhalation of as few as 10 organisms in the form of an aerosol can cause severe pneumonia.
In disseminated cases, characteristic focal necrotic lesions in various stages of evolution are scattered throughout the body. They are 1 mm to 8 cm and whitish yellow; they are seen externally as the primary lesions on the fingers, eyes, or mouth and commonly occur in lymph nodes, spleen, liver, kidneys, and lungs. In pneumonia, necrotic foci occur in the lungs. Although severe systemic toxicity may occur, no toxins have been demonstrated.
Symptoms and Signs
Onset of tularemia is sudden, occurring 1 to 10 (usually 2 to 4) days after exposure, with headache, chills, nausea, vomiting, fever of 39.5 to 40° C, and severe prostration. Extreme weakness, recurring chills, and drenching sweats develop. Clinical manifestations depend to some extent on the type of exposure.
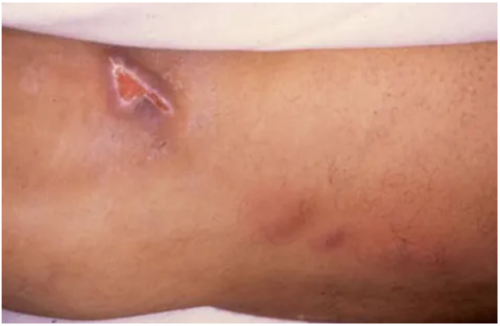
Within 24 to 48 h, an inflamed papule appears at the site of exposure (finger, arm, eye, roof of the mouth), except in glandular or typhoidal tularemia. The papule rapidly becomes pustular and ulcerates, producing a clean ulcer crater with a scanty, thin, colorless exudate. Ulcers are usually single on the extremities but multiple in the mouth or eyes. Usually, only one eye is affected. Regional lymph nodes enlarge and may suppurate and drain profusely. A typhoid-like state frequently develops by the 5th day, and the patient may develop atypical pneumonia, sometimes accompanied by delirium.
Pneumonic tularemia can occur after inhalation or by hematogenous spread from another type of tularemia; it develops in 10 to 15% of ulceroglandular tularemia cases and in about 50% of typhoidal tularemia cases. Although signs of consolidation are frequently present, reduced breath sounds and occasional rales may be the only physical findings in tularemic pneumonia. A dry, nonproductive cough is associated with a retrosternal burning sensation. A nonspecific roseola-like rash may appear at any stage of the disease. Splenomegaly and perisplenitis may occur. In untreated cases, temperature remains elevated for 3 to 4 wk and resolves gradually. Mediastinitis, lung abscess, and meningitis are rare complications.
Mortality is almost nil in treated cases and about 6% in untreated cases of ulceroglandular tularemia. Mortality rates are higher for type A infection and for typhoidal, septicemic, and pneumonic tularemia; they are as high as 33% for untreated cases. Death usually results from overwhelming infection, pneumonia, meningitis, or peritonitis. Relapses can occur in inadequately treated cases. One attack confers immunity
https://www.msdmanuals.com/professional/infectious-diseases/gram-negative-bacilli/tularemia
https://newbp.bmj.com/topics/en-gb/916
http://www.cfsph.iastate.edu/DiseaseInfo/disease-images.php?name=tularemia&lang=en