Ehrlichiosis / Anaplasmosis
Posted on 10 April 2023.
EHRLICHIOSIS and ANAPLASMOSIS
Signs and symptoms of ehrlichiosis typically begin within 1-2 weeks after the bite of an infected tick.
Tick bites are usually painless, and many people do not remember being bitten.
See your healthcare provider if you become ill after being bitten by a tick or spending time in grassy, brushy, wooded areas.
Early Illness
Early signs and symptoms (the first 5 days of illness) are usually mild or moderate and may include:
Fever, chills
Severe headache
Muscle aches
Nausea, vomiting, diarrhea, loss of appetite
Confusion
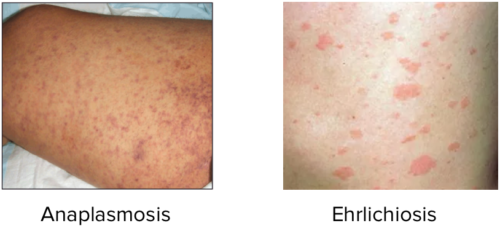
Rash (more common in children)
Rash
Up to 1 in 3 people with ehrlichiosis report a rash; rash is more common in people with E. chaffeensis ehrlichiosis and generally occurs more often in children than adults. Rash usually develops 5 days after fever begins. If a person develops a rash, it can look like red splotches or pinpoint dots.
Late Illness
If antibiotic treatment is delayed, ehrlichiosis can sometimes cause severe illness. Early treatment can reduce your risk of developing severe illness.
Signs and symptoms of severe (late stage) illness can include:
Damage to the brain or nervous system (e.g. inflammation of the brain and surrounding tissue (called meningoencephalitis))
Respiratory failure
Uncontrolled bleeding
Organ failure
Death
Risk factors for severe illness:
Delayed antibiotic treatment
Age: being very young or very old
Weakened immune system: such as those receiving some cancer treatments, individuals with advanced HIV infection, people who have received organ transplants, or people taking certain medications
Clinical features of ehrlichiosis and anaplasmosis are similar. Although some infections are asymptomatic, most cause abrupt onset of an influenza-like illness with nonspecific symptoms such as fever, chills, myalgias, weakness, nausea, vomiting, cough. headache, and malaise, usually beginning about 12 days after the tick bite.
Rash is uncommon in anaplasmosis. Some patients infected with E. chaffeensis develop a maculopapular or petechial rash on the trunk and extremities.
Ehrlichiosis and anaplasmosis may result in disseminated intravascular coagulation, multiorgan failure, seizures, and coma.
Both infections appear to be more severe and have a higher mortality rate in patients with compromised immunity caused by immunosuppressants (eg, corticosteroids, cancer chemotherapy, long-term treatment with immunosuppressants after organ transplantation), HIV infection, or splenectomy.
Anaplasmosis info
https://aem.asm.org/content/79/24/7583
Human Granulocytic Anaplasmosis (HGA)
is an infection caused by the intracellular bacterium Anaplasma phagocytophilum. As a tick-borne disease, the public health impact of HGA continues to increase with range expansion of the disease vector. The clinical presentation of HGA is often a non-specific febrile illness. The presence of leukopenia, thrombocytopenia, and mild hepatic injury are frequently noted on laboratory investigations, which can be important diagnostic clues in attaining an appropriate diagnosis. Herein we present three cases of HGA, highlighting the spectrum of disease by which HGA can manifest. Although each case has their unique features, we outline important shared clinical elements to facilitate an empiric diagnosis while definitive laboratory investigations are pending. Our case series further serves to highlight the critical importance of prompt antimicrobial treatment to reduce morbidity and potential mortality.
https://www.sciencedirect.com/science/article/pii/S2214250918301744#bib0030
Prevalence of Anaplasma bovis in Canadian populations of the Rocky Mountain wood tick, Dermacentor andersoni
As temperatures increase in Canada, the environment becomes more suitable for ticks and the season suitable for tick activity lengthens, so tick-borne diseases are likely to become more common in Canada. In addition to Lyme disease, four other tick-borne diseases (TBDs) have started to emerge and are likely to increase: Anaplasmosis; Babesiosis; Powassan virus; and Borrelia miyamotoi disease.